Tag
surprise medical bills
-
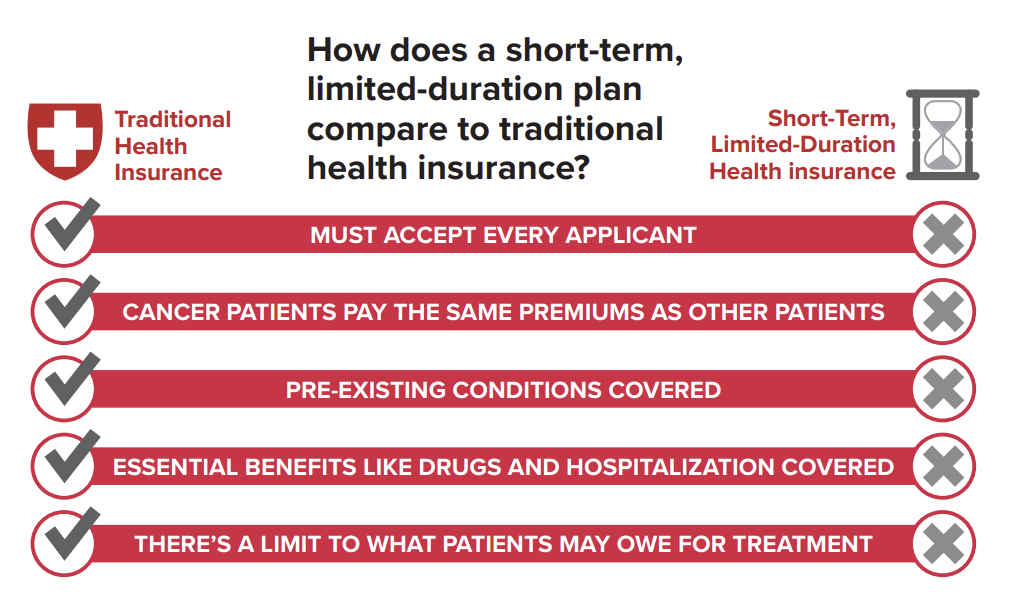
Proposed rules would protect consumers from junk insurance plans, surprise bills and medical debt
Junk insurance plans that don’t meet the standards of the Affordable Care Act are one of the biggest holes in…

-
Another lobbying battle looms on surprise medical bills
The unveiling of a new federal rule last week to prevent “surprise” medical bills is worth covering on its own…

-
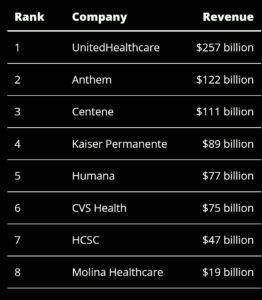
Expect more pushback from insurers and hospitals over rules to limit surprise bills
On July 1, the nation’s largest health insurer, UnitedHealthcare (UHC), stopped paying out-of-network claims when its fully insured members seek…

-
GAO report confirms the financially toxic nature of air ambulance fees
Over the past several years, health care journalists have done great work highlighting the problem of surprise medical bills. There’s…