Tag
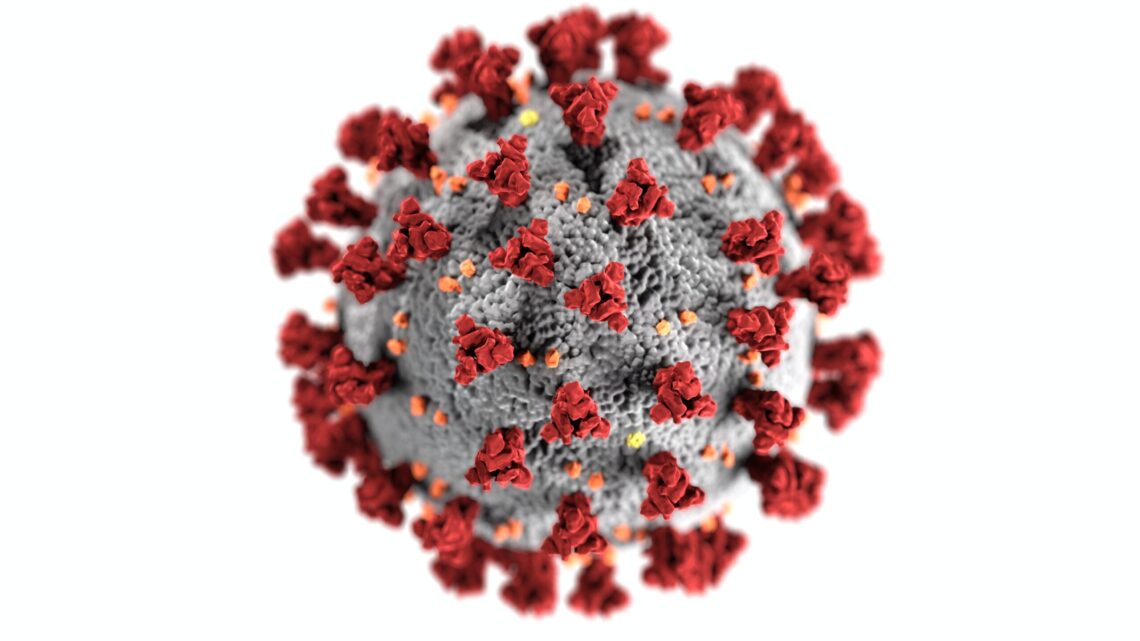
COVID-19
-
Is the Biden administration’s plan to revamp nursing home standards enough?
It took a pandemic and tens of thousands of deaths before most people became aware of just how bad circumstances were in…

-
Why journalists should report on wastewater
With an increasing number of states slowing the pace of reporting on COVID-19 cases, journalists should consider keeping an eye…

-
Hundreds of peer-reviewed papers have cited a retracted study on COVID-19
Amid the madness of spring to summer 2020, it was impossible to keep up with the influx of publications about…

-
Another brewing infectious disease threat and looking to COVID-19 for solutions
The threat of antibiotic resistance continues to grow in 2022. Reporters looking for new angles on how to cover this brewing…

-
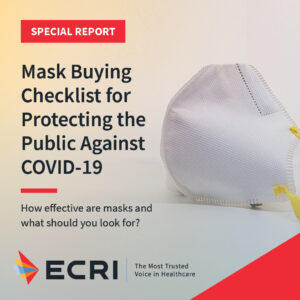
Avoiding “message fatigue” when reporting on masks and COVID-19
Trying to engage audiences when writing about obtaining and wearing appropriate masks to prevent the spread of COVID-19 can be…

-
Covering COVID-19 treatments: One journalist’s personal story and some resources
In mid-January, New York Times reporter Rebecca Robbins shared her personal story of hunting down the antiviral Paxlovid to successfully treat her…

-
Two new studies address fertility and COVID vaccines
One of the most persistent concerns about potential adverse effects from the COVID-19 vaccines has been whether they will affect…

-
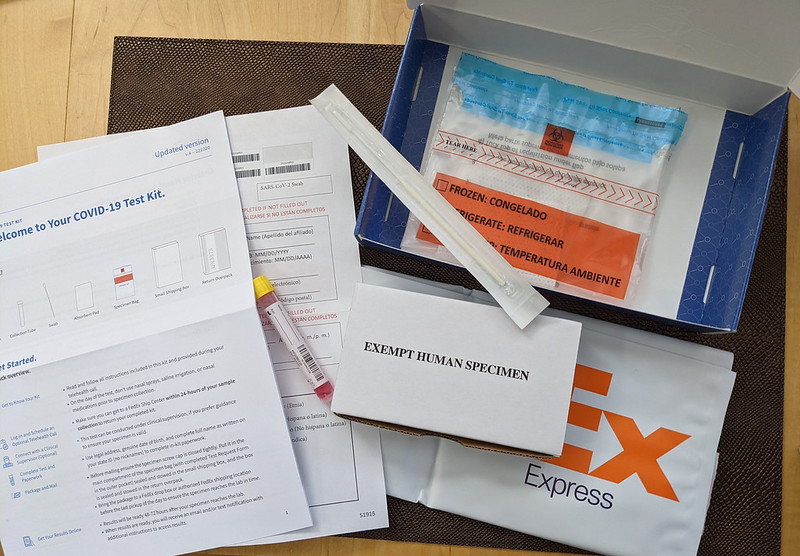
Covering rapid testing and resources
Rapid COVID-19 testing, how to get them and how to use are among the biggest pandemic stories. In the coming…

-
Mental health topics to explore in 2022
Almost two years of pandemic lockdowns, re-openings, retreats from re-opening, and coronavirus variants — and another COVID-19 winter upon us…

-
Understanding the CDC’s updated quarantine and masking guidance
On Dec. 27, the CDC significantly shortened isolation and quarantine times for people who have tested positive for the SARS-CoV-2…