Tag
COVID-19
-
Science magazine reporter Jon Cohen digs deep into history of coronaviruses
Science journalist Jon Cohen discusses how he reported on the history of coronaviruses and their link to SARS-CoV-2.

-
•
Parsing the deadly problem of low vaccination rates in nursing homes
In this webinar, hear why vaccination rates for COVID-19, RSV and even the flu remain low among nursing homes and…

-
How to cover this year’s worsening respiratory illness season
Respiratory illnesses are seeing an uptick in 2024. Here’s what you need to know to report on COVID, RSV, the…

-
•
Covering long COVID, the hidden epidemic
In this webinar, you’ll hear from a rehabilitation physician specialized in treating people with long COVID and a journalist living…

-
How to report on the COVID-19 uptick when the public says ‘meh’
COVID-19 cases have begun rising again as the new school year looms. Here are some fresh angles for covering the…

-
Science journalist: More evidence supports ‘spillover’ COVID-19 origin than lab leak
Science magazine reporter Jon Cohen shares his perspective on the ongoing controversy about COVID-19’s origin and advice for covering it,…

-
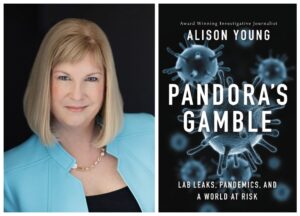
Webinar will focus on new book, the ‘lab leak’ theory and keeping an eye out for hazards
In an upcoming webinar with “Pandora’s Gamble” author Alison Young, we will discuss the seriousness of lab leaks and theories…

-
Loneliness and health inequity are post-COVID-19 stories to cover, reporter says
A Q&A with freelance writer Fran Kritz on covering the pandemic for NPR and story ideas after the global health…