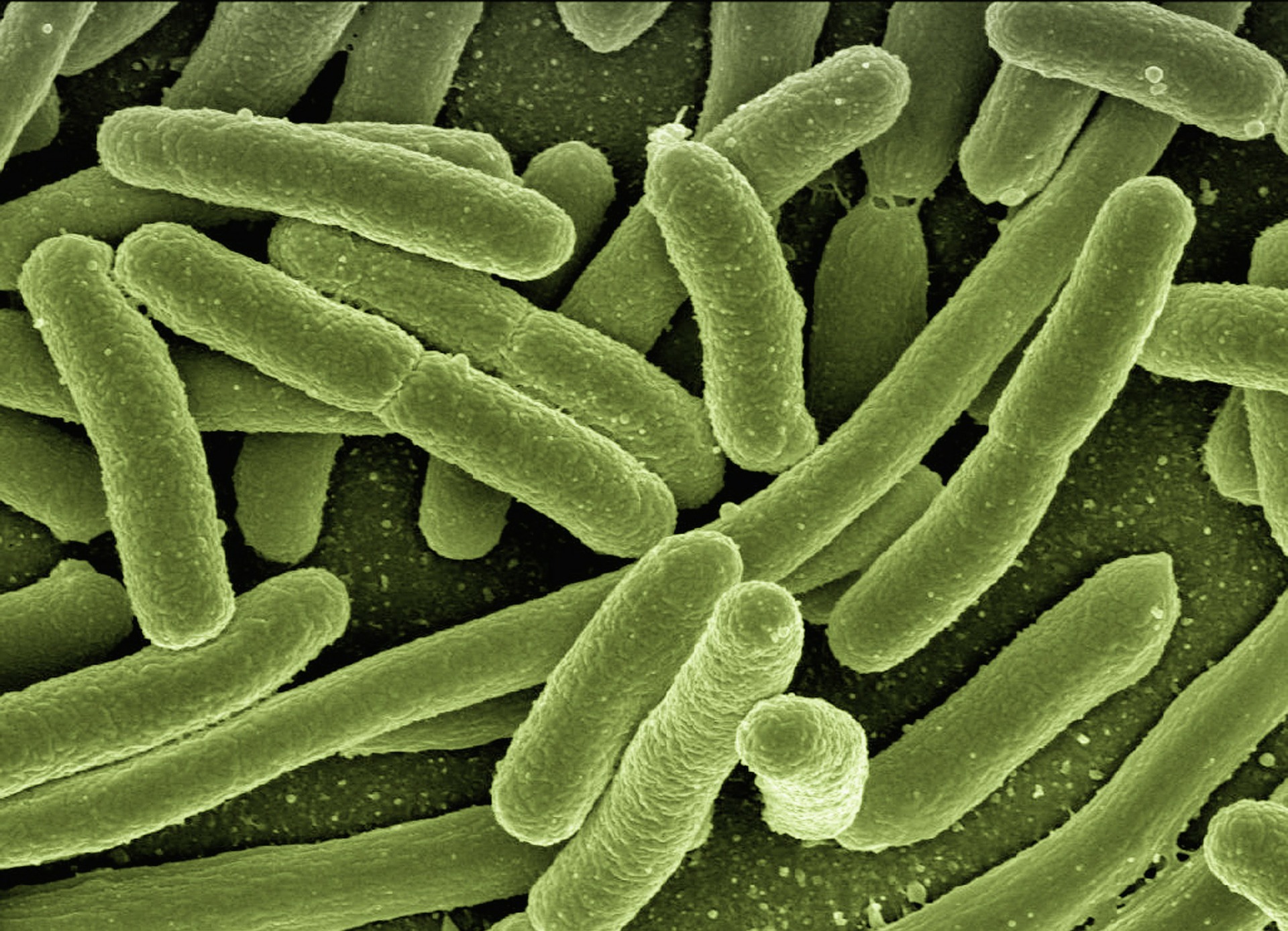
 The threat of antibiotic resistance continues to grow in 2022. Reporters looking for new angles on how to cover this brewing danger can look to efforts by public health advocates, drug company leaders and federal legislators, who are pushing for federal policies that encourage the development of new antibiotics. Their efforts come as two recent reports demonstrate that another potential global infectious disease crisis is percolating.
The threat of antibiotic resistance continues to grow in 2022. Reporters looking for new angles on how to cover this brewing danger can look to efforts by public health advocates, drug company leaders and federal legislators, who are pushing for federal policies that encourage the development of new antibiotics. Their efforts come as two recent reports demonstrate that another potential global infectious disease crisis is percolating.
One January 2022 report concluded that 1.2 million deaths globally were the result of drug resistance in 2019 — higher than previously understood. Another showed that the pipeline of new antibiotics to replace those that no longer work remains dangerously thin and likely won’t expand unless the federal government steps in like it did during COVID-19 with vaccines.
“Among the many sobering reminders of the COVID-19 pandemic has been the critical importance of public health preparedness,” Kathy Talkington, director of health programs at Pew Charitable Trusts, wrote in a Feb. 3 letter to a U.S. Senate committee in support of legislation to spur the development of new antibiotics. “While we were not aware of COVID-19 before its emergence, experts have been warning for decades about the threat of antibiotic resistance … Yet, their value to health care has been taken for granted; all the while, their effectiveness gradually diminishes.”
The CDC estimated in 2019 that about 35,000 people a year in the U.S. die from a drug-resistant infection, which is up from 2013 when the agency estimated about 21,000 were dying annually from a superbug. This is the latest national data available from the CDC.
Since then, antibiotic resistance has likely accelerated during the pandemic, as hospitals have been giving more antibiotics to hospitalized patients than necessary. In the fourth quarter of 2020, hospitals reported a 41% increase in infection events caused by bacteremia, bacteria in the bloodstream, and often drug-resistant pathogens, according to the CDC. The rise in infection was likely related to the large surge in COVID-19 patients admitted to hospitals who needed ventilators and catheters and other equipment to keep them alive, all of which could create opportunities for bacteria to enter the body.
“We’ve seen a rise in broad-spectrum antibacterial use nationwide during this pandemic,” Shruti Gohil, M.D., M.P.H., associate medical director of epidemiology and infection prevention at the University of California, Irvine School of Medicine, said in this November 2021 AHCJ article. And “there has also been a rise in multidrug-resistant organism infections, specifically” in hospitals.
On Feb. 14, the biotechnology industry released a comprehensive report on its most up-to-date estimates of the existing antibiotic pipeline, which found that there are 64 potential antibacterials under development, mostly in earlier stages of clinical trials. The lack of new potential drugs is tied to economics. Antibiotics are less lucrative than drugs for diseases like cancer and diabetes because unlike chronic illnesses, people only need to take an antibiotic for a few days.
“This is an ecosystem that’s fragile, failing and basically dying,” Evan Loh, CEO of Paratek Pharmaceuticals, a small biotech producer of an antibiotic, said of the antibiotics market.
The research and development situation with antibiotics is not unlike the research landscape with coronavirus vaccines before the pandemic. For almost two decades, researchers had been working on coronavirus vaccines, but there was little interest from the private market to invest in them until the pandemic. The federal government then stepped in with Operation Warp Speed, and within a year, COVID-19 vaccines were available to the public.
Congressional lawmakers have introduced several measures that could create the kind of economic incentives that were provided for the COVID-19 vaccine. One is the “21st Century Cures 2.0 Act” that would provide $11 billion to spur the antibiotics market. The government spent about $10 billion for Operation Warp Speed. Another is called the “Developing an Innovative Strategy for Antimicrobial Resistant Microorganisms (DISARM) Act” which would encourage hospital purchasing of new antibiotics. A third is the “Pioneering Antimicrobial Subscriptions to End Upsurging Resistance (PASTEUR) Act” which would build an economic model used in the United Kingdom to encourage antibiotic development. However, to date, no hearings have been scheduled for any of these bills.
For reporters looking for experts on this topic, check out this AHCJ tip sheet. Here are several additional experts to contact:
Infectious disease and policy experts
- Ramanan Laxminarayan Ph.D., M.P.H., is the founder and director of the Center for Disease Dynamics, Economics & Policy (CDDEP) and senior research scholar and lecturer at Princeton Environmental Institute; ramanan@cddep.org.
- Shruti Gohil, M.D., M.P.H., is the associate medical director of epidemiology and infection prevention at the University of California, Irvine School of Medicine; skgohil@uci.edu.
- Eli Perencevich, M.D., M.S., is director of Health Services Research & Development and Comprehensive Access & Delivery Research & Evaluation at Iowa City U.S. Department of Veteran’s Affairs Healthcare System) Center of Innovation in the Department of Internal Medicine at the University of Iowa Carver College of Medicine; eli-perencevich@uiowa.edu.
- Kathy Talkington, M.P.A., is the project director of The Pew Charitable Trusts’ Antibiotic Resistance Project; ktalkington@pewtrusts.org.
Academics
- Lance B. Price, Ph.D., is a professor at George Washington University’s Milken School of Public Health and founding director of the Antibiotic Resistance Action Center; Lprice@gwu.edu.
- Kevin Outterson, J.D., is co-director of Boston University’s health law program and executive director of CARB-X; mko@bu.edu.
- Brad Spellberg, M.D., is professor of clinical medicine and associate dean for clinical affairs at the University of Southern California Keck School of Medicine and chief medical officer of Los Angeles County-USC Medical Center; spellber@usc.edu.
- Anthony So, M.D., M.P.A., is professor of the practice and founding director of Johns Hopkins Bloomberg School of Public Health’s Innovation and Design Enabling Access Initiative and director of the strategic policy program of ReAct – Action on Antibiotic Resistance; aso5@jhu.edu.
Antibiotic development
- John Rex, M.D., is the chief medical officer and director at F2G and former expert-in-residence at the London-based Wellcome Trust. You can contact him through Maggie Servais: maggie@keybridge.biz.
- Evan Loh, M.D., is CEO of Paratek Pharmaceuticals and a former faculty member at both Harvard Medical School and the University of Pennsylvania School of Medicine. Reach him through Christine Fanelle: christine@scientpr.com.
Advocacy organizations
- Association for Professionals in Infection Control and Epidemiology is an over 15,000-member organization with a mission to advance the science and practice of infection prevention and control. Media contact: Aaron Cohen, aaroncohenpr@gmail.com.
- American Society for Microbiology is a 50,000-member organization that promotes infectious disease research, including antibiotic resistance; communications@asmusa.org.
- Antibiotic Resistance Action Center is based in the George Washington University Milken Institute School of Public Health. This organization brings together epidemiologists, microbiologists, communications experts, and policy experts to combat antibiotic resistance; araclab@gwu.edu.
- Infectious Disease Society of America is an 11,000-member professional organization that represents infectious disease practitioners and often sponsors reports about antibiotic resistance; TWilliams@MessagePartnersPR.com.
- Working to Fight AMR is the BIO industry’s advocacy group working on antibiotics. Reach the director Emily Wheeler via Maggie Servais, maggie@keybridge.biz.







