Tag
elderly
-
The older population is growing and becoming more diverse
The Administration for Community Living (ACL) has published its profile of older Americans 2021, an annual summary of critical statistics related…

-
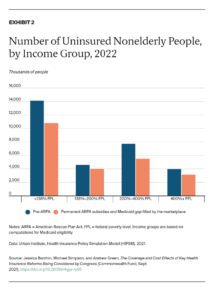
Report shows consumers could save even more on health insurance
Reporting on how much consumers will save on health insurance under the American Rescue Plan Act (ARPA) has never been…

-
Tips for reporting on what experts say could be a tough flu season for the elderly
As cases of the Delta variant start to wane, infectious disease specialists have a new concern this fall — flu…

-
Reporting on suicide among the elderly — a major public health issue even before the pandemic
The pandemic’s assorted pressures have caused a spike in suicidal thoughts among subsets of people, including older Americans whose risk…

-
Older health care professionals at risk during COVID-19 outbreak
Retired physicians, nurses and other health care professionals have been asked to volunteer for duty in the wake of the…

-
Simple language helps convey health information
As I was scanning posters during last spring’s American Society on Aging’s conference, I spotted one presentation that stopped me…

-
Elder abuse commonly committed by relatives, study indicates
Relatives, not strangers, may be the people most likely to take advantage of older adults, according to a new study…

-
Journalist, students dive deep into local elder abuse investigation
Tracy Breton, a Pulitzer prize-winning investigative and legal affairs reporter at the Providence Journal for 40 years, and now professor…

-
Report finds antipsychotic drug use still rampant in some nursing homes
Despite efforts to curb the use of antipsychotic drugs in nursing homes, about 20 percent of residents – more than…

-
Study documents the high cost of falling for older adults
Should health providers be doing more to screen for fall risk in older adults? New research seems to indicate that…