Tag
Aging
-
Why age bias has real world health effects
A new study found that ageist attitudes and negative self-perceptions of aging directly affect an older person’s physical and mental…

-
Webinar to explore cancer reporting without hype and with the right measure of hope
Experts on an upcoming AHCJ webinar on Wednesday, July 19, will discuss communication about cancer screenings and treatment.

-
Resilience factors in older women could hold key to better quality of life
Study finds older women with more education and less stress have more resilience in older age.

-
Poll shows most older adults use assistive tech to age in place
A new U.S. News survey finds that more seniors are adopting apps, wearables and services to help remain at home.

-
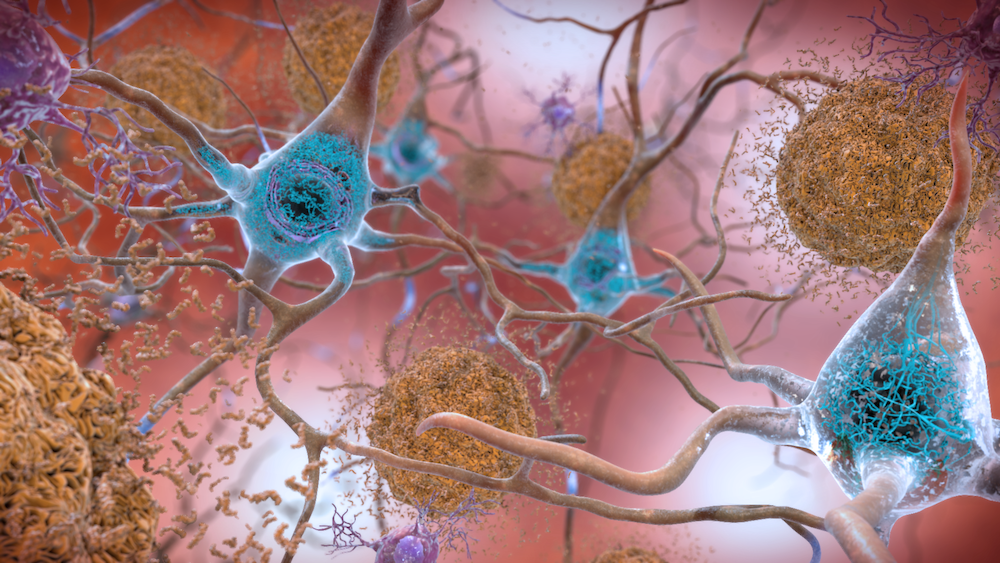
Medicare announces coverage of costly Alzheimer’s medication. That could mean high premiums for beneficiaries
Medicare coverage of new Alzheimer’s treatments will raise premiums and increase out-of-pocket costs for beneficiaries, new analysis finds.

-
Learn how to track vaccination rates among multigenerational households
In a deep-dive story for the Center for Public Integrity, a reporting team looked at the risk of contracting the…

-
Journalists can help shed light on COVID-19 vaccine schemes
It’s still difficult for many eligible older adults in parts of the U.S. to get COVID-19 vaccination appointments. And that’s…

-
Study shows racial differences in COVID-19 nursing home deaths
Racial disparities are glaringly obvious when examining COVID-19 caseloads, hospitalizations and deaths. A new study in JAMA Open looks at…

-
Are older lives less worthy in a pandemic?
You may have heard the comments from Texas Lt. Governor Dan Patrick earlier this week, when he said that the…

-
Tip sheet, article focus on creating a podcast about aging
Ever thought about starting a podcast? You’re not alone. There are an estimated 750,000 podcasts, and 30 million episodes available…