Tag
errors
-
Expert and author traces history of patient safety movement, suggests stories
Yes, there’s a lot going on these days. Impeachment. Potential war. The 2020 election. (Forget for a minute the cynic’s…

-
Advocate talks about progress on patient safety, offers story ideas
Lisa McGiffert is best known by journalist, health provider organizations and regulatory agencies, as the former director of the Consumers…

-
Annual list provides opportunities for stories on hazards in health care
The ECRI Institute every so often comes out with top 10 lists, and on Monday it issued its latest, focusing…

-
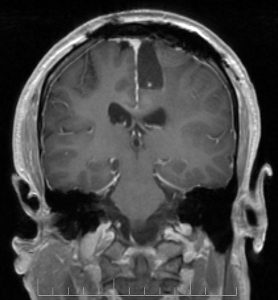
Why we should use caution when reporting on AI in medicine
Hospitals and health systems are jumping into artificial intelligence (AI) in an effort to help physicians better analyze images and…

-
•
Journalists learn about efforts to improve diagnostic process
If you’ve read Dr. Lisa Sanders’ “Diagnosis” column in The New York Times Magazine, you know the process of identifying…

-
Exploring ‘preventable harm’ and making it accessible to readers
Vox’s Sarah Kliff, who has an AHCJ Reporting Fellowship on Health Care Performance, is writing a series about fatal, preventable…

-
OIG: While adverse events are common, records of them aren’t
To draw attention to its ongoing monitoring of the incidence of adverse events in US hospitals and the accurate reporting…

-
•
Formula 1 pit crews inspire physicians
In American Medical News, Kevin O’Reilly examines a study of the lessons physicians have learned from the high-speed ballet of…

-
•
Canadians fight for disclosure of medical treatment
It took eight years, a whistleblower and intervention from a state commissioner to uncover a fatal medical error in a…