Category
Uncategorized
-
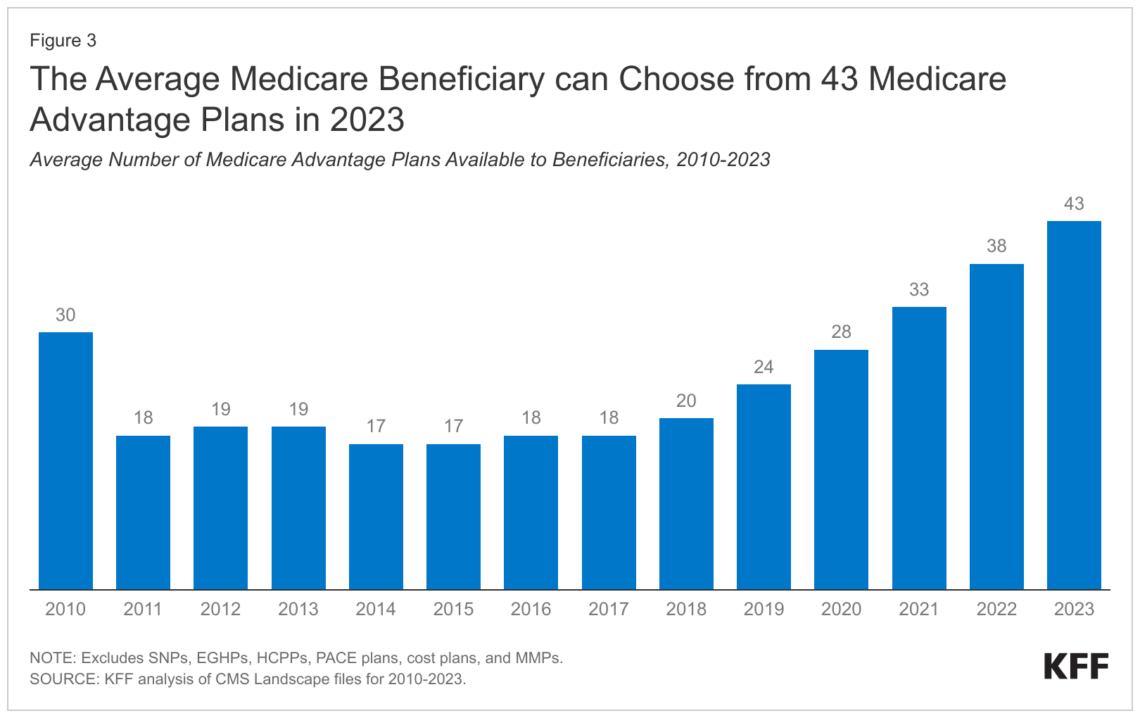
As open enrollment begins, older adults have questions about how to afford Medicare coverage
Many Americans ages 65 and up have difficulty affording Medicare premiums and prescription drugs. Journalists have an opportunity to help…

-
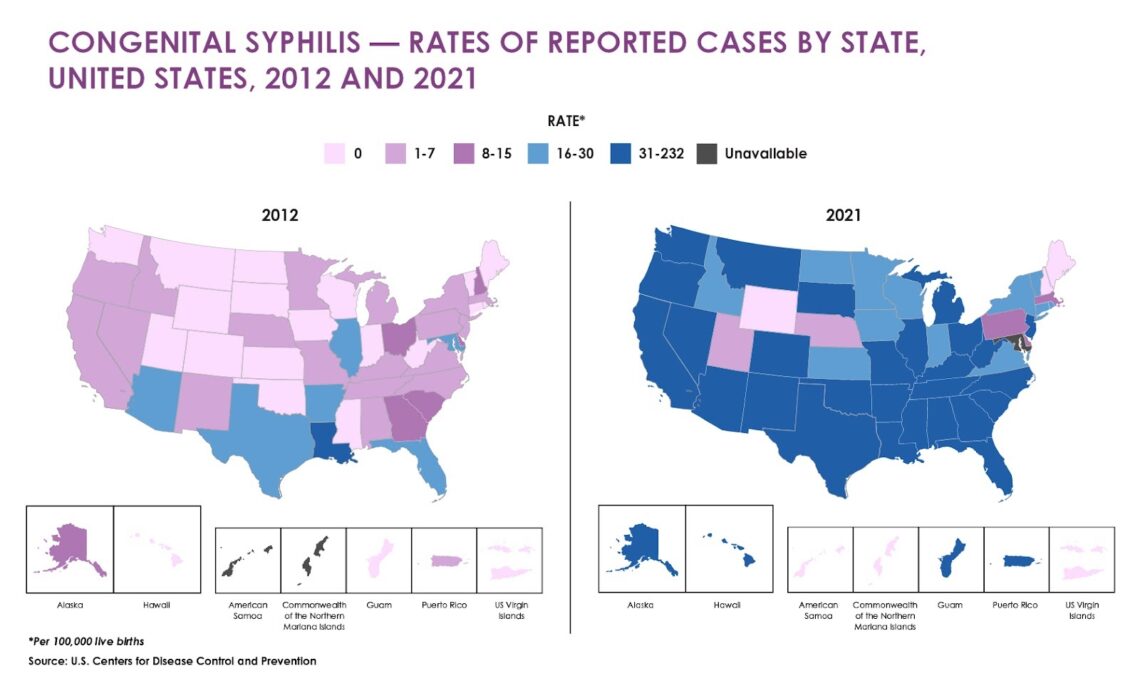
Tips for reporting on the syphilis crisis
Rising cases in newborns has brought renewed attention to an international syphilis crisis. As clinicians race to stem the spread,…

-
Why climate change matters for seasonal allergies and asthma
It’s not just your imagination; seasonal allergies are getting worse, partially due to climate change. Here’s why you should report…

-
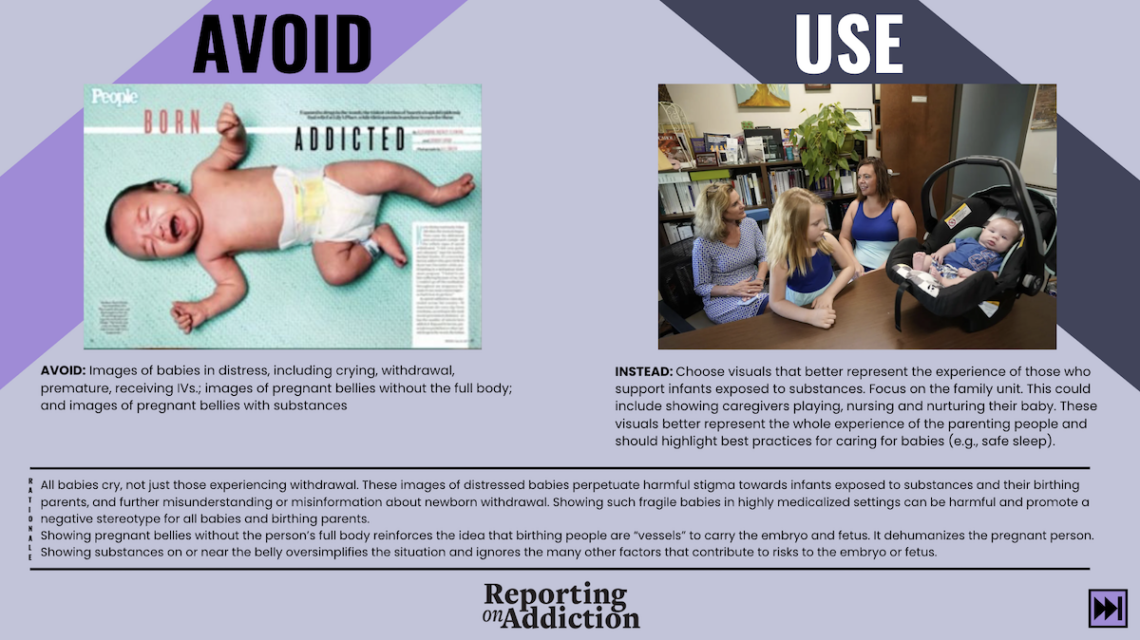
‘Offensive’ news about opioids in Appalachia prompts launch of website aimed at improving addiction coverage
Do you cover drug addiction in your community? If so, you should be aware of how, among other things, word…

-
Can practitioners still prescribe controlled medications via telehealth?
Should health care practitioners retain the ability to prescribe controlled medications to patients via telemedicine — perhaps without any in-person…

-
Keep your audience informed on the scarcity of children’s COVID-19 vaccines
Federal agencies have approved the latest COVID-19 vaccine for everyone 6 months and older; so why are some pharmacies still…

-
Fall summit strives to put homelessness on reporters’ radar as a health issue
The day-and-a-half event will take place Nov. 2-3 in Oakland, Calif., at the Waterfront Hotel – JDV by Hyatt. Registration closes…

-
10 tips for eliminating ageist language from your stories
Tips and ideas for reporting on older people and eliminating ageism, stereotypes and wrong assumptions about people over the age…

-
Johns Hopkins analysis of CDC firearms suicide data reveals grim milestone
The firearms suicide rate among Black teenagers surpassed the rate for white teenagers for the first time on record in…

-
Prior approval: Journalists and researchers show health insurers’ performance is abysmal
In the past year, journalists and health researchers have uncovered troubling facts about how health insurers fail members by delaying…