Proposals put forth last fall in a sweeping 34-page report from the President’s Council of Advisors on Science and Technology (PCAST) could jumpstart progress on patient safety — an area where only modest strides have been made in recent decades.
Notably for journalists, the expert panel prioritized requiring hospitals to publicly report patient harms — a step that is likely to face industry opposition but has long been advocated by watchdogs as a consumer right and a cornerstone for improvement.
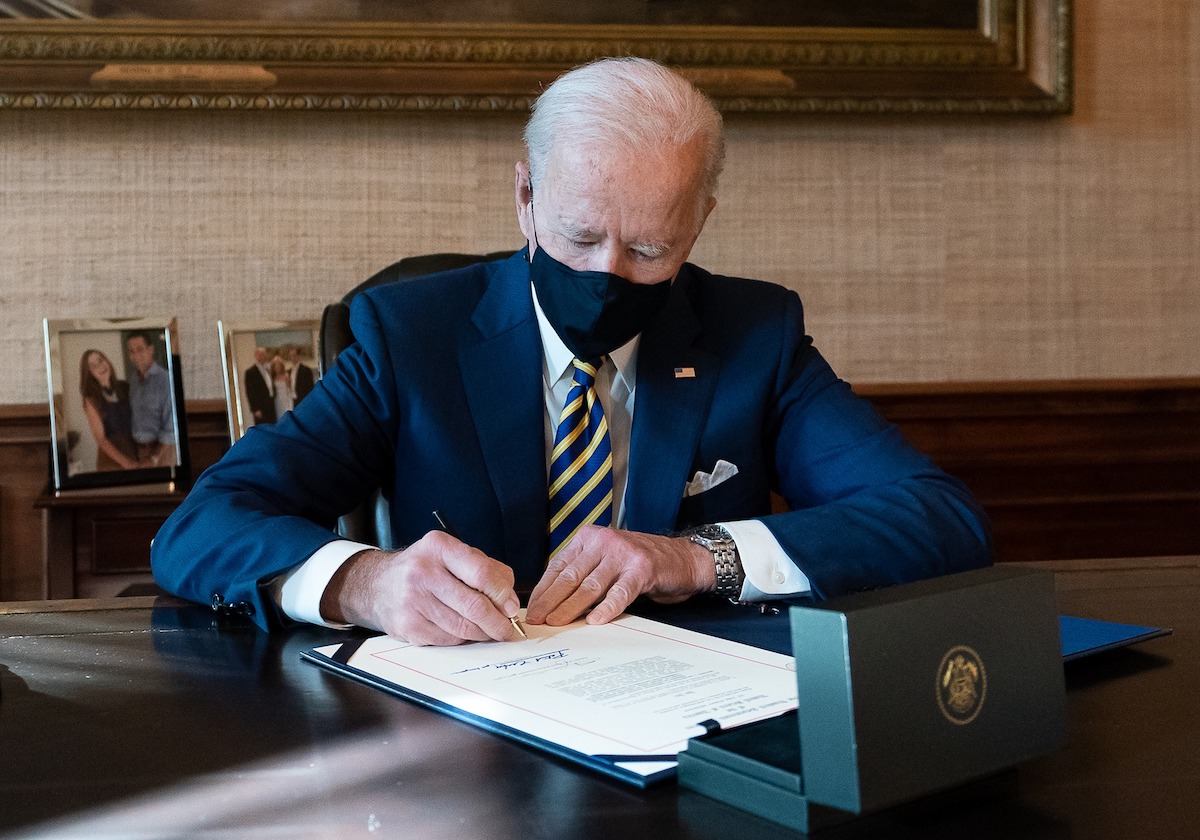
So far the recommendations have garnered scant media coverage, which means journalists have an opportunity to scrutinize them by outlining how they would affect the delivery of care, gathering reactions from patient safety experts, and reporting on whether President Joe Biden acts on them.
An indication of Biden’s plans may soon be at hand.
Advocacy group is ‘optimistic’

Michael Ramsay, M.D., chief executive officer of the Patient Safety Movement Foundation, an advocacy group, said via email that the White House in recent weeks has requested data on implementation costs and recoupment periods for health systems that have implemented some or all of the measures. The foundation’s founder, Joe Kiani, chairman and CEO of Masimo, a company that makes monitoring devices, co-led the PCAST working group that developed the recommendations.
“The feedback that we received from the White House was that President Biden was very supportive of the recommendations,” Ramsay said.
Ramsay said the queries suggest that the president might bring them up in the State of the Union address on March 7. Such financial details would be “of significant current concern” to Congress, he said.
However, Ramsay added that the foundation is optimistic that the administration will enact the measures in the six government-funded health care programs, which would not require congressional approval. Those programs are Medicare, Medicaid, the Children’s Health Insurance Program, TRICARE, the Veterans Health Administration, and the Indian Health Service.
Biden has long advocated for measures to curtail medical errors, including delivering a keynote speech at the foundation’s summit in 2015.
What the experts propose
The recommendations aim to create a federal patient safety infrastructure while holding individual hospitals accountable for implementing proven safety practices. They were crafted with input from researchers, hospital administrators and patient advocates.
The working group that assembled the recommendations “was truly impressive,” said Michael Millenson, a health care quality consultant and former journalist. He added that “the fact that this group of scientific advisors understood how important patient safety is” constituted “a breakthrough.”
Below are highlights from the report, which can be read in its entirety here.
Establish federal leadership.
- Boost the profile of patient safety, as the Biden administration has done for other causes such as cancer.
- Appoint a patient safety coordinator to oversee efforts of various federal agencies.
- Establish a public-private national patient safety team to investigate safety lapses and issue industry recommendations, along with a system to allow anyone to report safety events (the body would resemble airlines’ Commercial Aviation Safety Team, with experts in areas like safety science and human factors).
- Make the Veterans Health Administration and the Department of Defense health system into international models.
Mandate transparency.
- Require individual hospitals to publicly report “never events,” annually at first and then quarterly. Such incidents include harms from medication or surgery, diagnostic errors, hospital-associated infections and serious fall and pressure injuries.
- Require hospitals to communicate with families and “appropriate medical bodies” when patients are harmed.
- To compel hospitals to comply, use “strong tools” such as CMS’s Conditions of Participation for Medicare and Medicaid.
Transform Medicare payments to reward safe practices.
- Withhold payment for both primary care and harm-related care when a patient is harmed and a hospital hasn’t followed related evidence-based safety practices (current CMS policy withholds payment only for harm-related care and regardless of whether a hospital followed safety practices).
- Conversely, reward hospitals that implement evidence-based practices by paying for both primary and harm-associated care when a patient is harmed. Examples could include pre-surgery checklists; standardized procedures for the use of devices such as urinary catheters and respiratory machines; communication procedures for shift changes; and “just cultures” that encourage reporting of safety problems.
Address disparities.
- Require demographic data in public reporting in order to track harms in vulnerable populations.
- Monitor the impact of transparency and payment rules on safety-net hospitals and hospitals that serve patients with greater social and medical needs, and offer resources to help them adopt safe practices.
- Reward facilities that have excellent safety records and treat underserved populations.
- Add questions about bias to the Hospital Consumer Assessment of Healthcare Providers and Systems survey.
Lean into technology.
- Launch a 10-year research and development program to integrate technology in areas such as medication management, diagnosis, monitoring, and predicting the effectiveness of treatments.
- Create an “AI for Patient Safety Program” to encourage the deployment of validated artificial intelligence tools.
- Increase interoperability and create incentives for device makers to share data with researchers.
- Mandate inclusion of unique device identifiers in electronic health records to improve detection of device-related safety problems.
Significant hurdles
There’s a lot for journalists to pick apart. For example, the fact that technology figures prominently is no surprise given that two tech executives — Kiani and Microsoft Chief Scientific Officer Eric Horvitz — were at the helm.
Many details were left to federal agencies to figure out, and there was no price tag, although Horvitz and Kiani claimed at a public meeting last July (second video, 41:15) that safety investments will save money for both payers and providers.
Also, one working group member, Lisa Cooper, M.D., M.P.H., who leads the Johns Hopkins Center for Health Equity, said during the meeting that she advocated for a “deeper dive” into equity issues that didn’t happen.
The biggest hurdle could be industry opposition to mandatory public reporting, which has thwarted transparency initiatives since the Clinton administration. In its report, the President’s Council of Advisors on Science and Technology called the ongoing lack of a national system to monitor and learn from harms “a blight upon the U.S. government.”
In December, the American Hospital Association announced that it’s launching its own Patient Safety Initiative, including an effort to provide its members with “more real-time, nationally aggregated insights” on patient safety outcomes.
Hospitals have complained about financial pressures due to rising costs. However, working group members suggested that any burden on hospitals can be eased by automating the process with electronic health records, and noted that hospitals already track harms in order to comply with CMS Conditions of Participation.
“Many of us sit on boards of hospitals, and we know that hospitals already do this internally. They review every adverse event on a much more regular basis than even quarterly,” Kiani said.