Health care journalists have multiple story angles to pursue as states disenroll adults and children from Medicaid and the Children’s Health Insurance Program (CHIP).
In a new tip sheet, we report that on April 1, states began unenrolling members in both programs because the coronavirus public health emergency will end along with the continuous enrollment provisions that Congress passed in the Families First Coronavirus Response Act of 2020.
Washington Post’s national health care policy writer Amy Goldstein, explained the situation well, writing, “This Medicaid ‘unwinding,’ as it is called, is a reprise of a pre-pandemic practice of requiring low-income people to demonstrate each year that they qualified for the coverage.” The unwinding looms as the nation’s biggest health insurance disruption since the Affordable Care Act (ACA) became fully effective on January, 1, 2014, she added. Funding for the Medicaid and CHIP health insurance programs for the poor come from the states and the federal government.
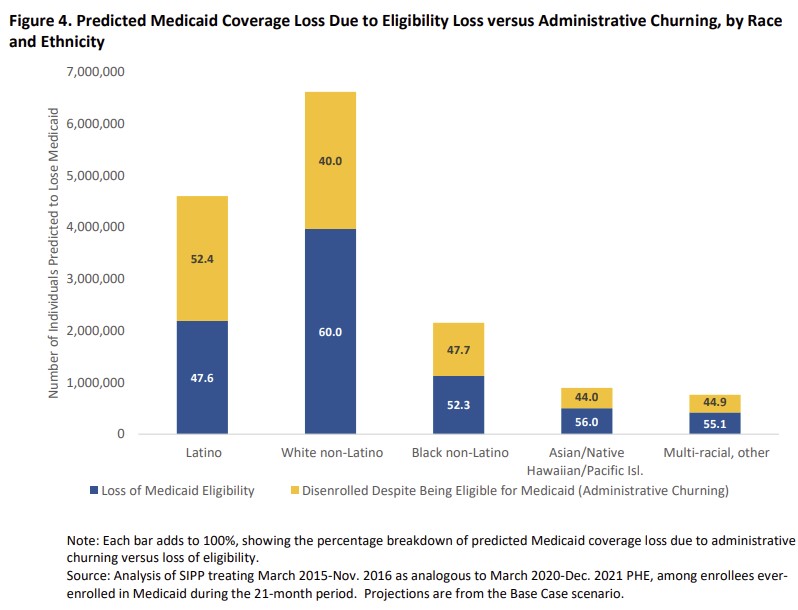
One story angle to consider is that the process of reviewing Medicaid coverage is likely to have a disproportionate effect on Black and Hispanic households, as Joseph Choi reported for The Hill newspaper last month.
In his report, Choi cited an analysis from The Commonwealth Fund showing that because Black and Hispanic Americans are disproportionately enrolled in Medicaid, they are at increased risk of losing coverage starting this month, when states begin to review all enrollees’ eligibility for coverage.
An analysis from the Kaiser Family Foundation showed that some 5.3 million to 14.2 million people could lose their Medicaid coverage and that an unknown number of them will find new coverage.
Estimates vary on how many adults and children will lose coverage. In a report last year, the federal Department of Health and Human Services (HHS) projected that 15 million Americans (or 17.4% of those enrolled in Medicaid and CHIP) would leave those programs. HHS’s Office of Health Policy published that report, “Unwinding the Medicaid Continuous Enrollment Provision: Projected Enrollment Effects and Policy Approaches.”
In that report, HHS predicted that 9.5% of Medicaid enrollees (8.2 million people) would leave because they are no longer eligible, and 7.9% (6.8 million) would lose coverage but still be eligible.
Here’s another angle: the disproportionate effect on 5.3 million children and an estimated 4.7 million young adults aged 18 to 34 who will lose coverage, according to aHHS report. As Choi noted, about one-third of those predicted to lose coverage are Latino (4.6 million) and 15% (2.2 million) are Black.
Journalists should remind their readers, viewers and listeners that about 33% (2.7 million) of those at risk of losing eligibility may qualify for premium tax credits under the ACA if they shop for health insurance on the marketplaces at www.healthcare.gov or if they visit the state-run ACA marketplaces in their states.
Among these 2.7 million people , most (60% or 1.7 million) may be eligible for zero-premium marketplace plans under the American Rescue Plan, HHS said. Some 5 million Americans who lose Medicaid may get other coverage, such as through an employer, HHS added.
For journalists interested in covering a “how they do it” angle on this topic, follow the example of Noah Weiland, a New York Times health reporter. In an article published earlier this week, Weiland wrote about his visit to Swope Health, in Kansas City, Mo., a federally funded network of health clinics. A group of Swope Health staff members were trying to call 19,000 Medicaid recipients to warn them about the impending loss of their health insurance, Weiland reported.








