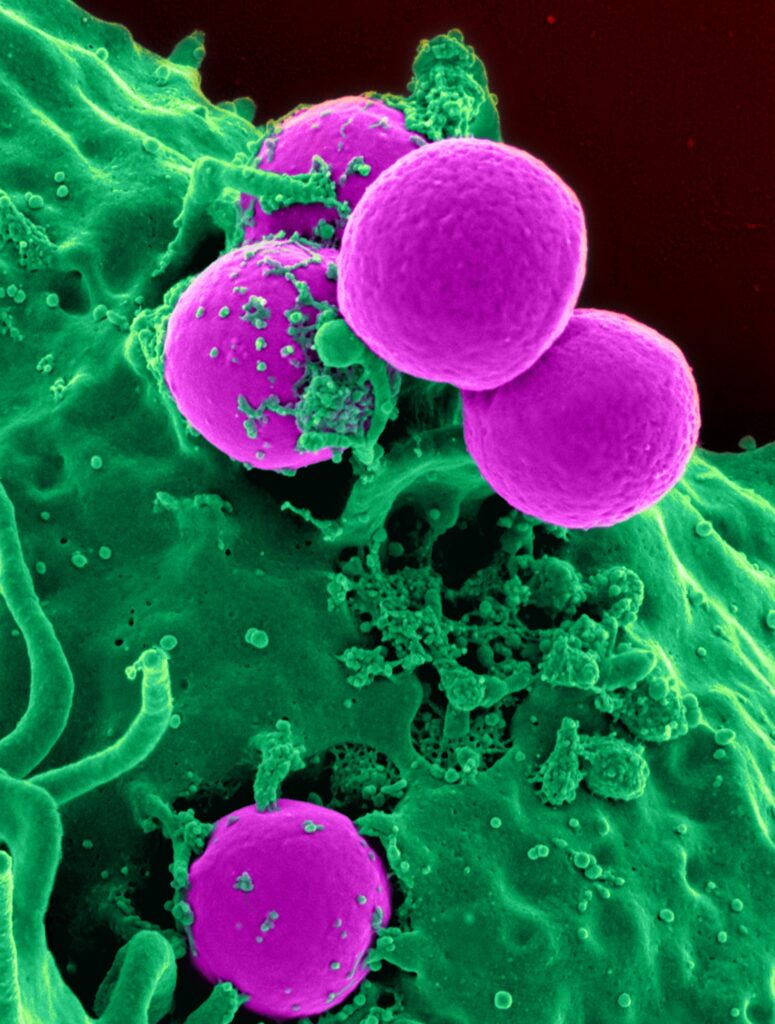
While the threat from the COVID-19 virus is fading in 2023, another pathogen is taking its place — microbes resistant to most if not all antibiotics and antifungals.
In the first three months of 2023, public health officials have reported four new health advisory alerts from bacteria and fungi — dubbed “superbugs” because of their resistance to drugs. They include Neisseria gonorrhea (causes the sexually transmitted disease gonorrhea), Candida auris (a fungus that can cause bloodstream infections), Shigella (causes severe diarrhea) and Pseudomonas aeruginosa (causes pneumonia and eye infections).
The superbug threat has been bubbling for decades as pharmaceutical companies have failed to develop new drugs to combat microbes that naturally gain resistance over time. The danger, especially among those who are immunocompromised, has grown even graver as the pandemic likely accelerated the development of new resistant pathogens, in part due to overprescribing of antibiotics and increased use of ventilators and catheters in hospitalized patients with COVID-19.
The rapid ascent of resistant bugs like C. auris is “unsettling,” Harry Skinner, CEO of AMR Action Fund, wrote in STAT, especially because “the U.S. — and the world has continually failed to take action against this threat.”
Valerie Gigante, Ph.D., team lead of the World Health Organization’s antimicrobial resistance division added: “Time is running out for us to bring new antibiotics to market and combat this urgent threat to public health. Without immediate action, we risk returning to a pre-antibiotic era where common infections become deadly.”
At the end of 2022, the U.S. Congress came close but failed to pass legislation, called the Pasteur Act, which would have created incentives for drug companies to develop new antimicrobials. The measure aims to create a guaranteed market for new antibiotics, which drug companies say is needed for them to invest in research and development for new drugs. (Because new antibiotics must be used sparingly, the market is considered too small for the hefty R&D price tag involved in developing new antimicrobials). The current state of political dysfunction means chances are low that anything will be enacted in Congress in 2023.
Health journalists can shed light on the need for policy changes by reporting on efforts at local hospitals, long-term care institutions and research institutions to monitor and combat these microbes. One way to find local stories is to look at the CDC investment map showing which institutions are actively working with public health officials on curbing antibiotic resistance.
Another story idea: lean into current pop culture interest in antimicrobial-resistant fungi linked to the streaming show “The Last of Us.” The HBO series is based on a video game about a deadly fungus, called cordyceps, that turns most of the earth’s humans into zombies. While fungi in the TV show only infect insects and are not a threat to humans, there are 19 other resistant fungi that are potential threats to humans, according to the WHO. Several drug companies are developing new drugs to fight them, but whether they will make it to the market without financial incentives is unclear. (See this Scientific American story on why the ‘Last of Us’ fungi isn’t one to worry about, but others are.)
For more story ideas and resources, check out my AHCJ tip sheet for reporting on antibiotic resistance.






