Health Beat
Monitoring the Pulse of Health Care Journalism
Ad
-
How to care for your mental health over the next few years
A second Trump administration will likely make health reporters’ jobs more chaotic (again). Here’s how journalists — and a psychologist…

-
New Medicaid work rules will challenge enrollees and states
Officials in 42 states have until 2027 to put new Medicaid work requirements in place so that millions can enroll…

-
JAMA Summit charts road map to reduce gun violence to record lows by 2040
Dozens of violence prevention leaders from across the U.S. convened in Chicago in March to discuss how to achieve “the…

-
Signs you’re dangerously overwhelmed as a freelancer — and what to do about it
During November’s Lunch and Learn, freelancers discussed their mental health challenges and shared resources to help.

-
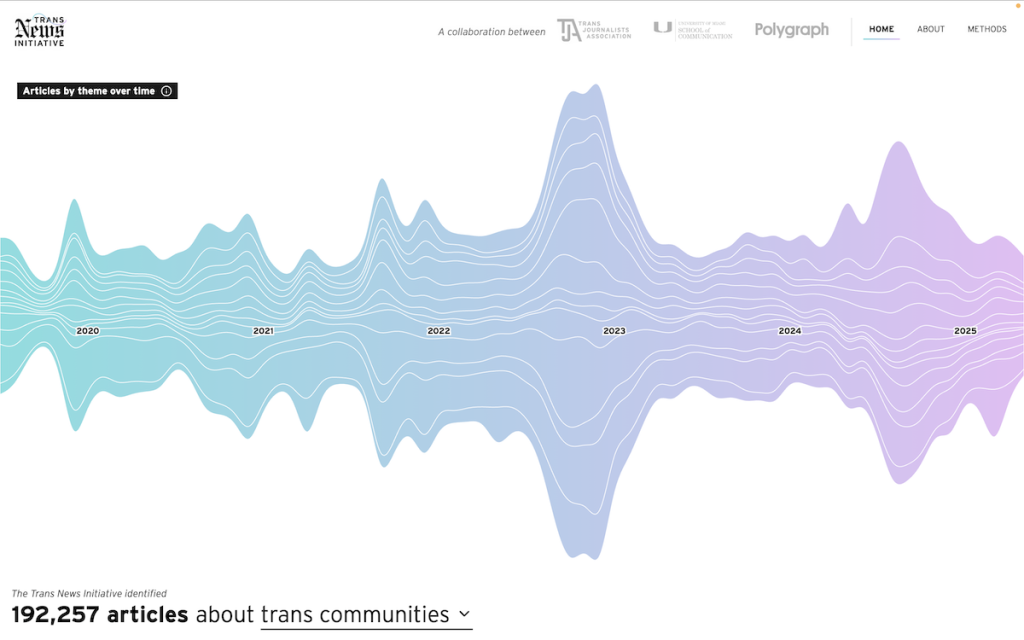
A new data tool for tracking trans news coverage
The Trans News Initiative aims to give reporters a clear view of the gaps and trends shaping public understanding of…

-
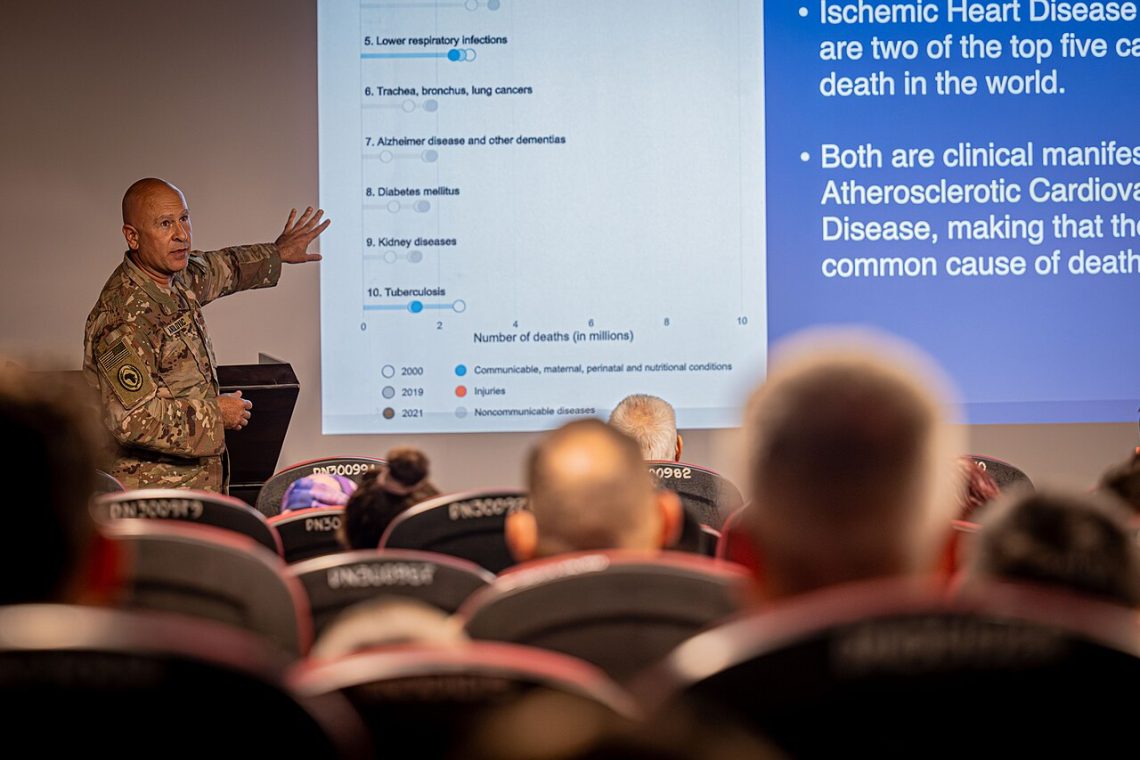
Get to know the parts of a medical conference
Making sense of a medical conference schedule can be overwhelming at first. Journalists, read this before you go.

-
Reports show health insurers skirt medical loss ratio rules
Health insurers increase health care costs and avoid paying rebates to consumers under the medical loss ratio rule in the…

-
Save the date for Health Journalism 2026 in Minneapolis
AHCJ and the Center for Excellence in Health Care Journalism is thrilled to bring Health Journalism 2026 to Minneapolis from…

-
Aging advocates brace for uncertain future
Longtime D.C. policy insider Bob Blancato briefs aging advocates on what to expect in federal aging policy for 2026 and…

-
New insights for health journalists from a climate communication research review
Many people don’t get important info about their health because it’s siloed as an environmental topic. Health journalists can help…

-
How to get quotes when scientists won’t talk on the record about climate change
Climate silence deepens among scientists affected by DOGE cuts. How do journalists get the quotes they need to inform their…

Featured Resources
Work the Health Beat.
Get exclusive news and training opportunities from AHCJ in your inbox once a week.