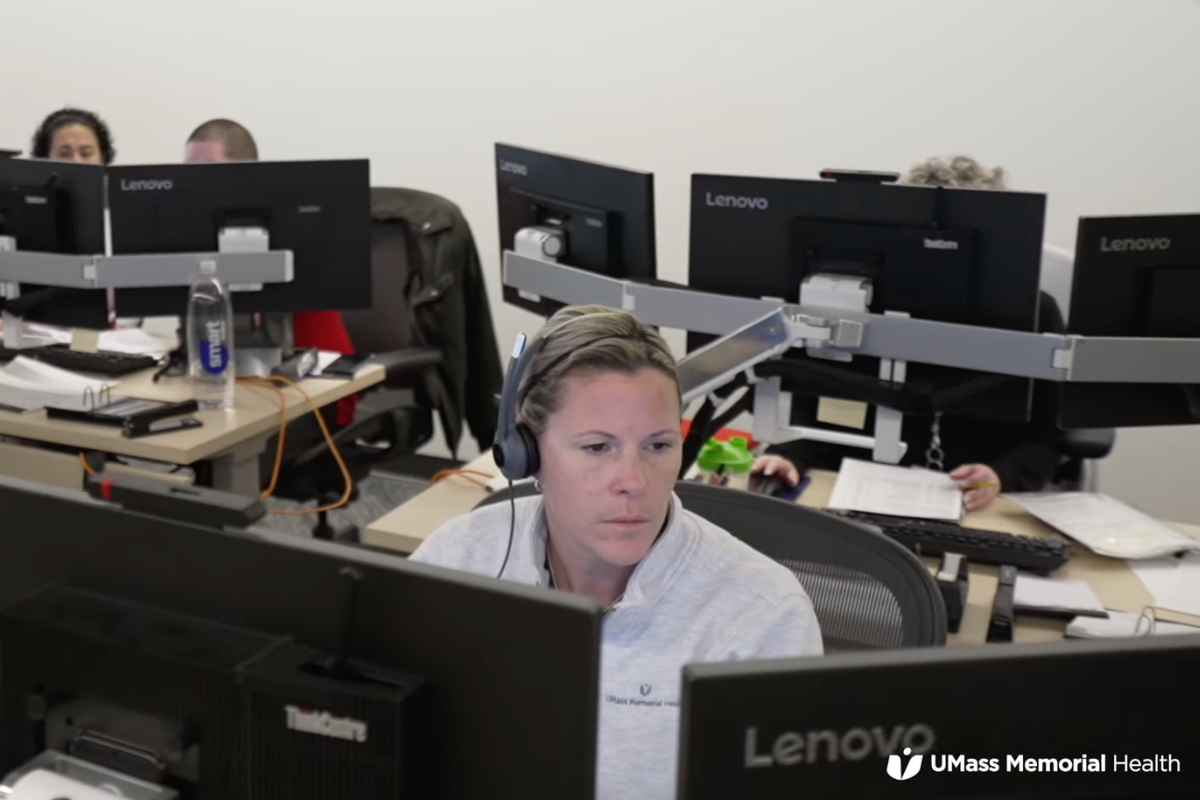
When the University of Massachusetts Memorial Health in Worcester opened its digital hub last fall, it provided a glimpse of what the future of remote care management could look like.
The 20,000-square-foot space, referred to as a “digital hospital,” merged many of the health system’s remote patient monitoring functions into one building. The structure is fully equipped with computers and monitors that allow experts to do remote clinical monitoring of patients in the intensive care units and their homes, keep an eye on patients at risk for falls and other safety concerns, and coordinate transfers of patients in and out of the hospital. It also allows other services like interpretation, and the structure has spaces for meetings and training sessions.
“When we think about a digital hub, it’s a setting that locates clinical caregivers and digital medicine capabilities to provide better care for patients, whether they’re in the inpatient setting, the ambulatory setting, or at home,” Eric Alper, M.D., senior vice president, system chief quality officer and chief clinical informatics officer at UMass Memorial Health, told Becker’s Health IT in February. “We’ve been trying to use digital strategies to help drive some of the more important system-level strategies that we have.”
It’s an interesting concept for journalists to watch and see if other medical centers follow suit, or as a jumping-off point for stories on remote patient management. For more on this topic, look for a session moderated by me on trends in hospital at home programs at Health Journalism 2025, AHCJ’s annual conference.
Features of the hub
One feature is the eICU, where clinicians monitor approximately 150 intensive care unit beds around the clock for patients in the UMass system and a few from other locations. Cameras and other equipment at every ICU bed allow clinicians to see and communicate with patients and give recommendations to care teams at the bedside.
“We are using high-level technology and software to determine if patients are decompensating or not, and how best to respond to those decompensations,” said Eric Cucchi, the director of eICU operations, in a video tour of the facility. The eICU is staffed by intensivists, medical doctors from specialties including pulmonary, critical care medicine and anesthesiology, and by advanced practice providers who have experience in critical care.
The eICU is most active at night, when the majority of physicians go home, Alper told Becker’s. If a nurse encounters an emergency such as a sudden drop in blood pressure, they can press a button that immediately connects them to an eICU physician via two-way video communication, the article noted.
Experts also monitor hospital inpatients on less acute wards, and those discharged to hospital at-home programs, gathering biometric data and providing health care coaching to reduce readmission rates and emergency department visits. Through a subacute rehabilitation at home program, care typically delivered in skilled nursing facilities is now able to be provided in the home with remote connections from patients to caregivers and some in-person home visits.
Remote monitoring is also conducted from the center for patients needing 1:1 observation due to risk of a fall or elopement. Patient care assistants at the digital hub watch up to six patients each to ensure safety. If they note any behaviors or safety concerns, they can sound an alarm in the patient’s room or contact a nurse on the ward.
Transfers, interpreters and more
Through the hub’s Transfer and Access Center (TRAC), employees facilitate transfers for patients coming from community hospitals in Massachusetts or beyond, and work with eICU colleagues to pave the way for critical care patients transferring to the medical center and some of UMass’ community hospitals. TRAC also hosts a toxicology consult service and telestroke service, and works out patient transfers with colleagues who operate Life Flight/helicopter patient transport services.
Also housed in the building are interpreter services. Clinic spaces in the medical center are equipped with tablets that can translate information into 250 languages, most on a 24/7 basis. For some of the more common languages, such as Spanish, the iPad will connect directly to one of the medical center’s interpreters, who operate out of 16 video-enabled and soundproof booths.
And, recognizing the need for employees to recharge during breaks, the building houses a meditation room and small gym as stress-relief spaces.
Resources:
- How UMass Memorial’s digital hub is redefining patient care – Becker’s Health IT.
- UMass Memorial creates digital hospital to centralize care and provide patient assistance throughout Central Mass – Worcester Business Journal.
- Tour the new digital hub at UMass Memorial Health – YouTube video.
- Remote patient monitoring the next wave in telehealth – AHCJ blog post from 2021.