When it comes to health care disparities and cardiovascular disease (CVD), the divide widens early. A spate of studies published recently illustrates how social factors influence CVD outcomes from our earliest years.
When it comes to health care disparities and cardiovascular disease (CVD), the divide widens early. A spate of studies published recently illustrates how social factors influence CVD outcomes from our earliest years.
For example, a report published in Pediatrics found that the increased obesity prevalence among U.S. adolescents is happening almost entirely among those in low- and middle-income families. Smoking, diet quality, and physical activity levels also tracked with household socioeconomic status for these children, based on the NHANES data used in the study. The only equal-opportunity metabolic derailment among teens in the United States appears to be prediabetes and diabetes. Risk factors for CVD overall declined for adolescents from 1999 to 2014, but significantly so only for those from high-income households.
Obesity has many contributing factors, including a genetic component. But even that factor falls under the influence of a child’s home environment from the early years, according to results published in JAMA Pediatrics. By age 4, twin pairs born in Wales and England in 2007 experienced a higher apparent genetic component to obesity if they grew up in homes with features of an obesogenic environment. Factors affecting the obesogenicity of the home environment include food availability and type of food, media use, and opportunities for physical activity. Genetics and environment became inseparable for these children as social factors under parental control involving food availability and media consumption acted against a genetic backdrop.
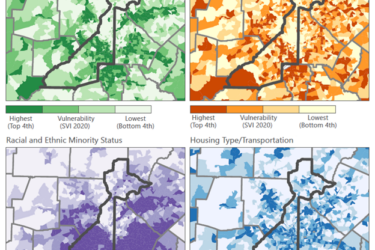
Children who are born with a CVD, i.e., congenital heart disease, fare far worse if they have a “high social risk,” the experience of social determinants that interfere with recovery from procedures to address their original condition. According to a report published in The Journal of Pediatrics, even a single social risk factor can undermine a child’s optimal recovery after interventions. Risk factors identified as highly relevant for these children include being a Medicaid recipient, having racial or ethnic minority status, and living in a high-poverty area. The takeaway from the study is that even children whose chances for a good recovery experience a deterioration in those odds if even a single social risk factor is present and fare worse than their counterparts without that risk factor.
A close-up look at California children with congenital heart disease confirms these findings. In results published in the Journal of the American Heart Association, investigators identified Hispanic ethnicity as factor in poor outcomes compared to outcomes for white, non-Hispanic children. Having private insurance and a mother with a high education level emerged as protective factors. In keeping with NHANES data, the characteristics of the infants in this study had a “minimal role” in how babies born with congenital heart conditions fared at 1 year. It was all about the social factors determining their health outcomes.
References and contacts
Jackson SL (at the CDC), Yang EC (Davidson College), Zhang Z (CDC). Income Disparities and Cardiovascular Risk Factors Among Adolescents. Pediatrics. 2018 Oct 17. pii: e20181089. doi: 10.1542/peds.2018-1089. [Epub ahead of print] PubMed PMID: 30333131.
Schrempft S (University College London; UCL), van Jaarsveld CHM (Radboud University Medical Center), Fisher A (UCL), Herle M (UCL), Smith AD (UCL), Fildes A (University of Leeds), Llewellyn CH (UCL). Variation in the Heritability of Child Body Mass Index by Obesogenic Home Environment. JAMA Pediatr. 2018 Oct 1. doi: 10.1001/jamapediatrics.2018.1508. [Epub ahead of print] PubMed PMID: 30285028.
Demianczyk AC, Behere SP, Thacker D, Noeder M, Delaplane EA, Pizarro C, Sood E (all duPont Hospital for Children). Social Risk Factors Impact Hospital Readmission and Outpatient Appointment Adherence for Children with Congenital Heart Disease. J Pediatr. 2018 Oct 23. pii: S0022-3476(18)31368-4. doi: 10.1016/j.jpeds.2018.09.038. [Epub ahead of print] PubMed PMID: 30366772.
Peyvandi S (USCF), Baer RJ (UCSF), Moon-Grady AJ (UCSF), Oltman SP (UCSF), Chambers CD (UCSD), Norton ME (UCSF), Rajagopal S (UCSF), Ryckman KK (University of Iowa), Jelliffe-Pawlowski LL (UCSF), Steurer MA (UCSF). Socioeconomic Mediators of Racial and Ethnic Disparities in Congenital Heart Disease Outcomes: A Population-Based Study in California. J Am Heart Assoc. 2018 Oct 16;7(20):e010342. doi: 10.1161/JAHA.118.010342. PubMed PMID: 30371284.