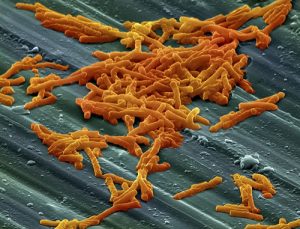
Potentially deadly Clostridium difficile (C. diff), which sickened an estimated half million Americans one recent year, has gained notoriety as a hospital-acquired infection.
Patients who have taken antibiotics face an elevated risk of acquiring the diarrheal disease, and the majority of infections occur in health care facilities, research has shown.
Not everyone infected with C. diff is a patient in a hospital or nursing home, and researchers trying to get a better understanding of cases acquired in community settings. They have concluded that antibiotics prescribed by dentists may be contributing to the spread of C. diff, which in 2011 killed more than 29,000 people in this country alone.
Primary care dentists write about 10 percent of all antibiotic prescriptions filled by pharmacies each year. That adds up to about 26 million prescriptions annually, according to federal data.
Concerns about antibiotic resistance and the spread of C. diff have fueled calls for responsible antibiotic use among medical providers in recent years. Researcher Stacy Holzbauer, an epidemiology field officer for the Centers for Disease Control and Prevention and the Minnesota Department of Health, told Medscape Medical News that dentists might not be as well-informed about the potential harms of antibiotic overuse,
Holzbauer and colleagues interviewed 1,626 people with community-acquired C. diff., and 926 reported they had been prescribed an antibiotic within three months of their illness; with 136 (15 percent) saying they had gotten the prescription from their dentist. The respondents came from five Minnesota counties and had acquired the disease between 2009 and 2015.
“I think the biggest issue is that dentists have been left out of the conversation because no one really recognized how large the dental prescribing was in the greater scheme of things, especially when it comes to outpatient prescribing,” said Holzbauer, who discussed her findings in a presentation at IDWeek 2017. The annual joint meeting of organizations including the Infectious Diseases Society of America (IDSA), which was held last October in San Diego.
Holzbauer said more study was needed to determine whether the Minnesota results could be generalized nationally.
Last year, Lauri Hicks, director of the Office of Antibiotic Stewardship at the Centers for Disease Control and Prevention raised similar concerns. Hicks urged dentists to follow evidence-based medical practices when prescribing antibiotics. “With data showing that 30 percent of all outpatient antibiotic prescriptions are unnecessary, it’s crucial that healthcare providers across all specialties commit to improving antibiotic prescribing in their individual practice settings,” she wrote.
“Due to barriers in data collection, it’s unclear exactly how much unnecessary antibiotic prescribing takes place in dentistry. However, there is concern that unnecessary and inappropriate prescribing is common in dental offices,” Hicks added.
To learn more about antibiotic prescribing practices and antimicrobial stewardship in the oral health world, check out this new AHCJ tip sheet.






