Looking for a local angle to cover antibiotic resistance?
Reporters can find potential stories by looking at the Centers for Disease Control and Prevention’s newly released antibiotic resistance investment map which provides details on superbug cases in states and CDC efforts to contain their spread.
Among the potential stories are cases of the antibiotic-resistant fungus Candida auris, found in Connecticut and Oklahoma, a reduction of a dangerous bacteria, carbapenem-resistant enterobacteriaceae (CRE), at health care facilities in Michigan and the expansion in the number of states capable of conducting whole-genome sequencing in suspected food poisoning cases.
“There has been a tremendous amount of investment by Congress and federal agencies to improve our [antibiotic resistance] capacities,” Michael Craig, senior advisor for antibiotic resistance coordination and strategy at the Division of Health Quality Promotion at the CDC’s Center for Emerging Zoonotic and Infectious Diseases, said during a December AHCJ webcast. “To localize this [for journalists], I would point out the investment map where you have lots of information about CDC’s specific investments locally.”
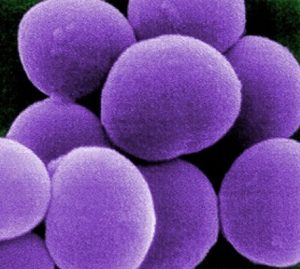
Twelve families of potentially lethal bacteria have become resistant to drugs that treat infections like pneumonia, blood infections, gonorrhea and food poisoning, according to the World Health Organization. The result has been a rising death toll from these resistant “superbugs.” By 2050, 10 million people could die from superbugs worldwide, if nothing changes.
The CDC is working to change the deadly trajectory through the National Strategy to Combat Antibiotic Resistance launched in 2015, Dr. Michael Bell, a physician and deputy director of the division of healthcare quality promotion at the CDC, explained during the AHCJ webcast. The CDC received additional funding from Congress – more than $160 million annually – for the program which included increasing the number of laboratories nationwide that can identify a case of a deadly bacteria before it has time to spread within a hospital or health care system to other patients.
“Before, we used to wait to see if there were a cluster of infections … before going in an intervening,” Bell said. “Now we aren’t waiting. We go in as soon as there is a single [antibiotic-resistant] infection.”
Other aspects of the strategy include ensuring health care systems are using the best antimicrobial resistant strategies, such as taking out catheters faster and working with the academic, private and international sectors to support work in developing new antibiotics, diagnostic and other medical tools for inhibiting antibiotic resistance.
Bell laid out some of the innovations the CDC has invested in, including pilot projects to use the microbiome (the healthy bacteria living in our guts and skin) to combat resistance, to developing surfaces that could be used in medicine that are resistant to any bacteria growth. While there aren’t any new blockbuster antibiotics expected on the market imminently, the CDC is working with Biomedical Advanced Research and Development Authority within the Department of Health and Human Services to fund accelerated development of antibiotics and diagnostic tools.
Bacteria are ever evolving, and therefore antibiotic resistance is an inevitable aspect of medicine. The best that public health officials can do is work to slow down the rise and the spread of deadly drug-resistant superbugs to ensure current antibiotics still work for most people and to give researchers enough time to find new ways to kill resistant germs, said Bell.
“People like to talk about preventing antimicrobial resistance, but that’s really not the goal,” Bells said during the webcast. “Our goal is to slow it down as much as we can so the antibiotics that we have keep working. Just inventing a new antibiotic is not a silver bullet. Every antibiotic that has been invented has had resistance show up very quickly soon after it is marketed, so we need to be thinking here about how do we preserve what we have got and also set things up so we preserve new developments, new antibiotics in the future and continue to make use of them.”
For more information:
- AHCJ Webcast: Covering Antibiotic Resistance in a Post Antibiotic World.
- What Reporters Need to Know About Antibiotic Resistance: An AHCJ Tip Sheet
- Video: Researchers: Overuse of Antibiotics Can Make Drugs Less Effective
- Center for Infectious Disease Research and Policy’s Antimicrobial Stewardship Project
- The World Is Running Out of Antibiotics – A Pew Charitable Trust Analysis of the Antibiotic Pipeline
- Antibacterial Agents in the Pipeline – A World Health Organization report
- Unnecessary Prescribing of Dental Antibiotics May Be Adding to C. Diff Cases
- Want to Beat Antibiotic Resistance? Rethink that Strep Throat Remedy
- Are Phages Our Best Bet Against Antibiotic Resistant Bacteria?








