Tag
nonprofit hospitals
-
Tip sheet: Nonprofit hospitals are gaming the system at patients’ expense
So far this year, hardly a week goes by without an article or report on egregious actions by nonprofit hospitals.…

-
Start digging: AHCJ’s hospitalfinances.org website is back online
Hospitalfinances.org, a site AHCJ launched in 2018 to provide free, searchable financial information on nonprofit hospitals across the United States,…

-
Nonprofits, tax breaks and getting hospitals to keep people out
Kaiser Health News and Capital News Service have been publishing a series called “Baltimore’s Other Divide” – the state of…

-
Brill reminds New York AHCJ members to follow the money
AHCJ New York members gained a unique look this week into how journalist, author, and businessman Steven Brill researched and…

-
•
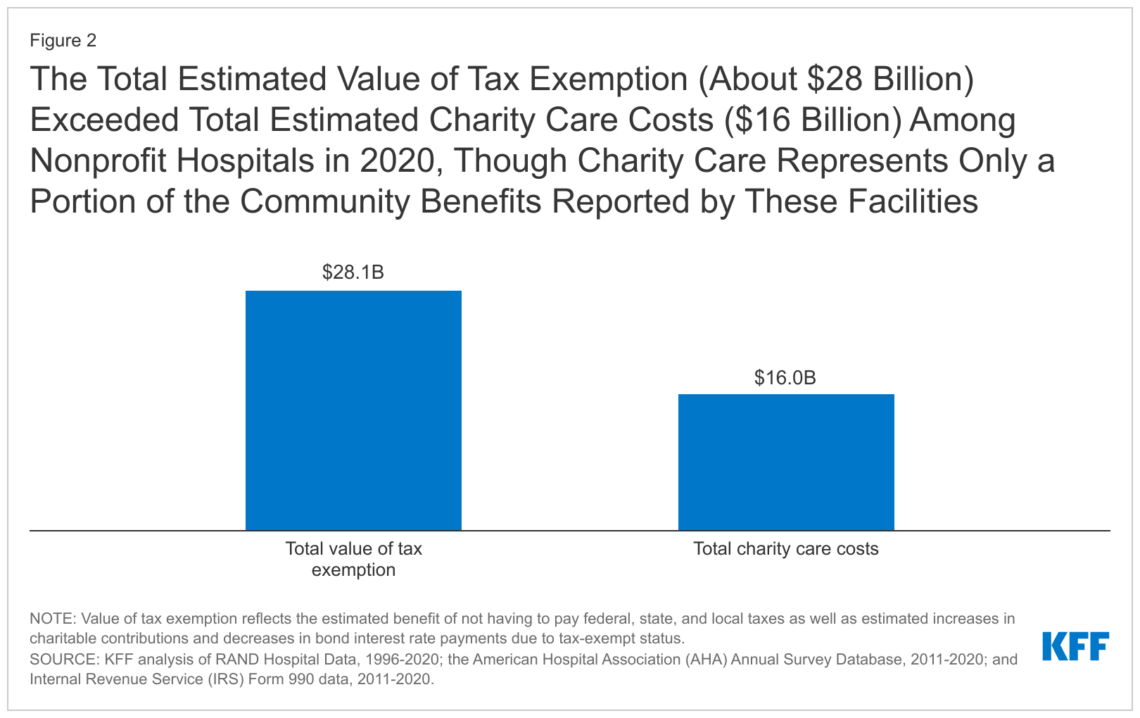
Public hospitals, not nonprofits, shoulder burden of charity care
Writing in the Contra Costa Times, Sandy Kleffman reports that while nonprofit hospitals in the East Bay are given millions…

-
•
Cash-strapped Ill. goes after hospitals’ nonprofit status
A New York Times article written by Bruce Japsen, an independent journalist writing for the Chicago News Co-Op, digs into…

-
•
Uninsured face delays, increased risks en route to long-term care
Writing for Heart & Soul, Yanick Rice Lamb offers up a comprehensive take on the special challenges patients and hospitals…

-
•
Reporter digs into nonprofit hospital CEO pay
At The Atlanta Journal-Constitution‘s M.B. Pell has assembled a look at CEO pay at local nonprofit hospitals. Pell hits hard…

-
•
Wash. hospital executive salaries may threaten nonprofit status
KUOW’s John Ryan, who has been using public records to investigate pay for nonprofit hospital executives, dove deeper into the…

-
•
Nonprofit hospitals pay country club dues for execs
In what would seem a logical follow up to last year’s piece on hospital salaries, KUOW’s John Ryan has used…